In the realm of healthcare, efficiency and productivity are paramount. In fact, in the NHS 2023/2024 priorities and operational planning guidance it quotes recovering productivity and improving whole system flow as critical to achieving its goals.
Yet, like an ocean liner navigating turbulent waters the NHS often finds itself slow to move when it comes to implementing productivity initiatives.
With a vast network of hospitals, clinics, and primary care facilities serving tens of millions of patients, it’s no wonder that effecting change within such a complex bureaucracy can feel akin to steering a behemoth ship. While some degree of deliberation and caution is understandable the NHS’s sluggishness in embracing productivity improvements is considered to be cause for concern.
Make changes, monitor impacts, move forward.
Moreover, the NHS’s hierarchical nature and centralised decision-making processes further reduce its overall response speed in implementing solutions to productivity challenges. Minor decisions take a path through layers of bureaucracy before even being trialled; resulting in delays and inefficiencies that impede progress. While centralised control can provide uniformity and standardisation across the healthcare system, it can also stifle creativity and innovation at the local level, where frontline staff are often best positioned to identify and address productivity bottlenecks.
Yet, amidst these challenges, there is a valuable lesson to be learned: failure is not a completely negative outcome. In fact, failure can serve as a catalyst for learning and improvement, provided that lessons are learned from the experience and shared openly with stakeholders. Transparency and accountability are essential components of any successful productivity initiative, as they create a culture of continuous improvement and innovation.
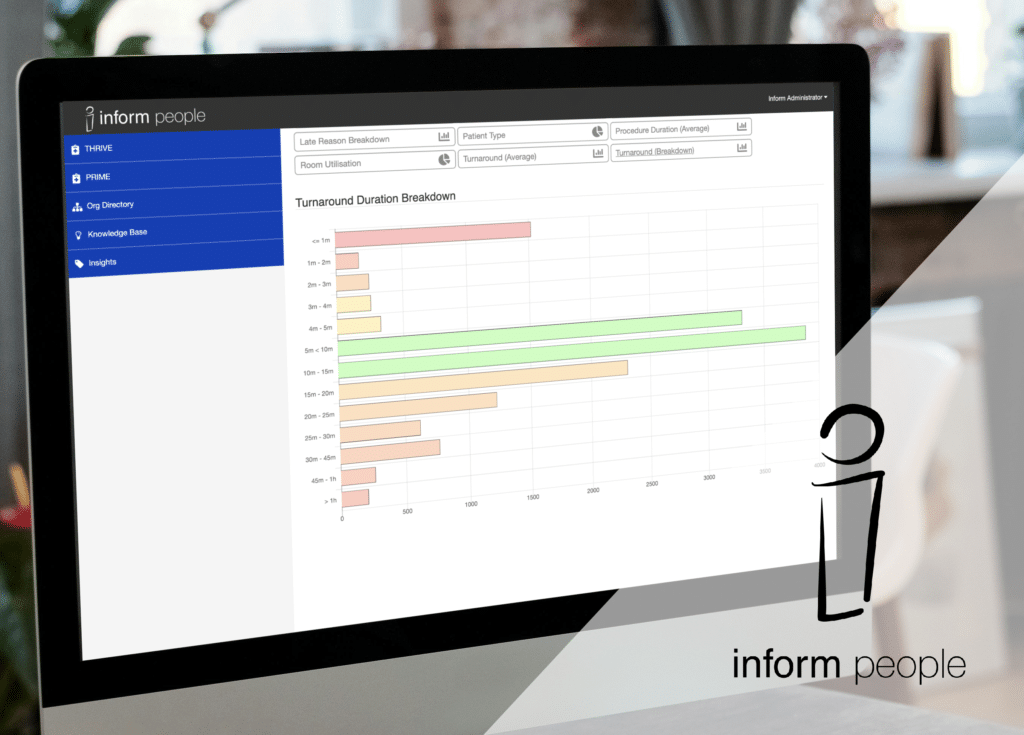
With THRIVE, Inform People’s time and list tracking tool, there is the flexibility to notice trends and make frontline changes – implemented on a local level at short notice – then also monitor the impacts with ease for the duration of any testing. Change can be trialled and judged on its effectiveness without requiring months of deliberation. Easy access to reporting tools allows a decision to be made quickly as to whether the change was successful or not, then the change can be reverted if ineffective or escalated up for wider testing and judgement if performance has improved.
Moving forward, the NHS must adopt a more agile and adaptive approach to productivity improvement, one that embraces experimentation and iteration rather than clinging to outdated models and previous practice. This requires a shift in mindset at all levels of the organisation, from senior leadership to frontline staff, towards a more entrepreneurial and risk-tolerant culture.
Another iceberg to navigate when considering productivity improvement in the NHS are data silos and their impact on wider performance. Since the introduction of the Data Protection Act 2018 (GDPR) the NHS has found itself struggling to share key information from one location or department to the next. An issue that should have been dealt with over 6 years ago still remains today and will need direct input if it is to change.
As THRIVE contains no patient information – just procedure types, points and timings – and can produce detailed, regular reports; data can be shared between trusts, networks and departments with ease. This allows for benchmarking performance and improves communication within networks. If all parties are using the same system and communicating the same type of information, it becomes clear where problems lie and who the best performers are. We can enable the sharing of best practice between consenting neighbours without having to navigate the icy waters that the Data Protection Act brought with it.
In conclusion, while the NHS may currently resemble an ocean liner in its approach to productivity improvement – slow and resistant to change – there is hope on the horizon. By embracing a culture of innovation, transparency, and continuous improvement, the NHS can cruise the waters of productivity more effectively, delivering better outcomes for patients and staff alike. Failure is not the end, but rather a stepping stone on the path to progress.
It’s time for the NHS to set sail towards a more agile and efficient future.