Recently we had a short article published in the HSJ – an opportunity to put forward Inform People’s ideas and experience as providers of technological solutions within the healthcare sector.
You can read the original article here: Time to Rethink Data Collection
With a limited word count, however, there was so much more we wanted to say; to expand on and to support with additional details, especially when exploring exactly how THRIVE is the solution that should be implemented to achieve the goals outlined. So that is just what this blog post will do.
Time to rethink data collection
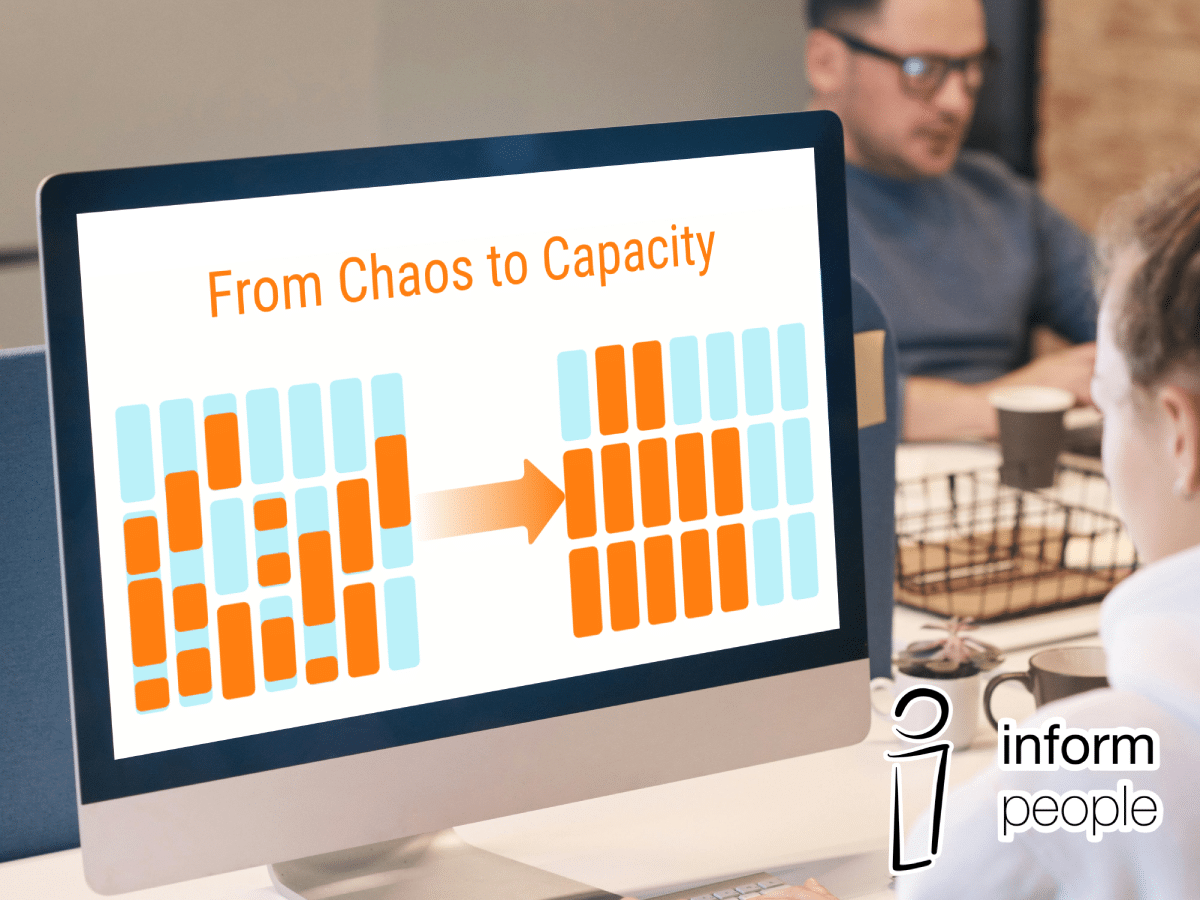
While aiming to improve NHS diagnostics and outpatient services, there is no shortage of data. However, there is a shortage of insight. The problem is shifting the focus of what data needs to be studied in order to maximise operational efficiency.
Working directly with a variety of hospitals we have seen that there is no single process that every team uses to collect information – the same information that is vital to the reports they are expected to produce regularly to support the hard work they are doing and to justify their productivity. Often we have seen that, prior to implementing THRIVE, there are both difficulties in extracting the information from where it is collected or that the data points that would be useful are not collected at all.
Too often, data collection has centred solely on the patient, but when looking at productivity, it’s about the hospital activity around them. A narrow lens ignores important activity happening around patients: the operational reality that defines how effectively services are running. Without capturing that, the data reflects only half of the picture.
These are the data points that could be fundamental in transforming the way that hospitals run to provide even better care for the population. THRIVE is specifically set up to record patient-free operational data and most importantly it is designed to be extremely light touch for the daily inputs whilst still revealing a wealth of information when reviewed.
The invisible work
Across the NHS, clinical teams are working under intense pressure, yet the data used to represent their activity is often disconnected. Turnaround time between patients, delayed session starts, and the impact of late cancellations all shape daily capacity and flow, but they are only partially recorded and rarely analysed.
For newcomers to THRIVE: a quick explanation. THRIVE is a website that gets a tailored setup and set of logins for each hospital department and the rooms within. Room accounts can manage list activity, Monitors build lists in advance, and Admins can view reporting. It is a streamlined platform that is set up to record activity in each room in a department with a simple Start/Stop button and a series of drop-down lists. Specifically designed with usability in mind to take as little time as possible to use and to keep healthcare professionals focused on the job at hand, whilst also capturing their activity. By recording the start and end times of each procedure and adding small additional details like Late Start reasons and Cancellation data if applicable, THRIVE is able to present core metrics like turnaround time and total list utilisation in a standardised, comparable and accessible way.
Data points may record that a patient was seen, the procedure priority type, or what medication they were given, but often fail to capture why the session started 20 minutes late, how this impacted turnaround times, or where capacity was lost or made up elsewhere in the day. These missing details are not minor; they are often where the most significant performance opportunities lie.
Clinical ≠ operational
Part of the problem is the systems used. Clinical reporting tools are excellent at capturing diagnoses, procedures, and outcomes, but they were never designed to reflect operational dynamics. It is a case of trying to answer productivity and workforce planning using systems built for patient care documentation. It is no surprise that the results are incomplete and difficult to utilise effectively.
For real progress, clinical data should be separate from performance data, especially for analysis. It means ensuring that operational flows, not just the clinical moments, are captured, allowing identification of patterns, highlighting constraints, and emboldening the scaling up of work.
That is why THRIVE has been built, and not to replace other important patient focused systems, but to sit alongside them without needing to double up on data input and to keep the resulting information collected free from identifying factors and GDPR hurdles.
It is not just about DNAs
One of the focuses in performance conversations is the focus on Did Not Attend (DNA) rates. While reducing DNAs is important, and for some trusts, this could be the productivity solution, DNA rates only explain a fraction of lost capacity. Yet, if the focus is solely on them, it might leave more actionable productivity improvements unexplored.
While we stand by this paragraph and its place in our original article, we also need to make a point that DNAs are extremely important to record properly. Cancellations and delays caused by non-attendance affect productivity for the whole week, every room and its utilisation is impacted each time a procedure does not go ahead. There will be a multitude of ways to tackle attendance that sit outside THRIVE, which hospitals are already trialing. The place where THRIVE comes in is by monitoring the impact of those methods by having a baseline in place and recording the ongoing daily activity to see the changes (either good or bad) that occur while trying to boost attendance rates.
There is also the ability, through knowing a department’s current DNA rate to implement strategies of overbooking or weighting and allocating certain procedure types to times of day or certain days of the week which might allow for better attendance rates too.
There are options to rework how sessions are structured, how rooms and equipment are shared, and how staffing affects throughput. Delays caused by hospital or patient cancellations, overrunning, staffing gaps and equipment issues can have as much impact as DNAs and also need to appear in reports.
Change requires visibility
NHS teams across the county are actively trying to innovate, with new scheduling models, overbooking strategies, and room configurations. When improvements do happen, they are often undocumented, stay local, and fail to inform system-wide learning.
One benefit that Inform People are proud of in our work via THRIVE is that we do not just deliver the technology and leave teams to use it. We are regularly in conversations with the people using THRIVE: to provide them with additional point-in-time reporting, facilitating meetings where senior teams share their best practice and outcomes, and then feeding all of these results back into future development of the product.
Thanks to working so closely with hospitals, THRIVE has been able to expand beyond the Endoscopy departments where it was first used and into Imaging, Radiology and Respiratory, with the potential to work effectively in many more departments in the future.
This is a critical gap. With no structured way to track changes or share outcomes, progress remains fragmented and siloed. Every trust ends up solving the same problems independently: a huge waste of time, resources and potential.
THRIVE also has an online global reporting functionality so that the most senior users can see all the hospitals under their care in real time too.
Productivity pressure is only growing
The 10-Year Health Plan makes the stakes clear: the system must “urgently resolve the NHS’s productivity crisis”. The national target? To deliver a 2 per cent year-on-year productivity gain for the next three years. That level of improvement is impossible if relying on only the existing reporting systems and the blind spots of the past. Sustained productivity gains demand better visibility, faster learning, and more targeted operational insight.
There is also the growing burden of reporting itself. NHS teams are asked to produce ever more detailed reports for national bodies. Yet, the action and problem-solving still happen at a local level. Meaning the same information is passed through multiple hands and reinterpreted and reformatted repeatedly. This duplicates effort and increases the risk of errors and flawed assumptions.
In summary
A shift in thinking is needed. Patient-focused data collection is important, but if unit productivity is the goal, focus must shift to the system around them. The tools to do this already exist, but need to be embraced nationally. What is needed now is a willingness to modify practices and take a leap towards a more efficient organisation.
Does your hospital need THRIVE? Get in touch with us today to organise a demonstration.